How a return to normal will impact some Indiana Medicaid members
During the COVID-19 federal public health emergency, due to federal requirements, Indiana Medicaid members were able to keep their coverage without interruption.
The most recent federal spending bill ended Medicaid coverage protections, which means Indiana Medicaid is returning to normal operations.
Eligibility redetermination actions began in April 2023, with a 12-month plan to return to normal operations.
Many of these redeterminations are done automatically based on information the state has available. In some situations, the state of Indiana will need to ask the member for information about themselves and their family, such as current address, employment status and income, age and family size.
Jump to section
What can members do?
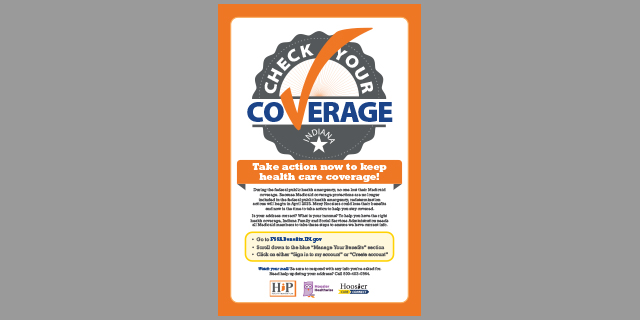
Anyone who is currently in one of Indiana Medicaid’s health coverage programs, including the Healthy Indiana Plan, Hoosier Healthwise, Hoosier Care Connect or traditional Medicaid, should take action now to help stay covered.
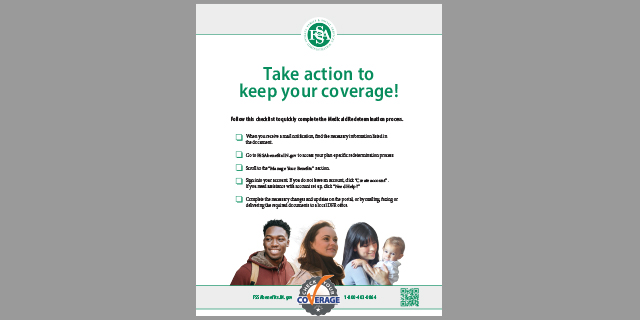
To help keep you covered, or help you find the right coverage for you and your family, the Indiana Family and Social Services Administration needs all Medicaid members to take these steps to ensure we have current information.
- Go to FSSABenefits.IN.gov
- Scroll down to the blue “Manage Your Benefits” section
- Click on either “Sign in to my account” or “Create account”
- Check that your contact information is accurate
- Call 800-403-0864 if you need assistance
- Then watch your mail! Be sure to respond with any information you’re asked to provide
- Benefit Portal tools:
- Click here for a flyer on how to navigate FSSABenefits.IN.gov
- Click here for a flyer on how to report a change
- Click here for a flyer on how to upload a document
- Click here to view a short walkthrough video
- Click here for videos showing how to:
- Change notification preferences
- Managing your user account
- Redetermination response process
- Upload documents
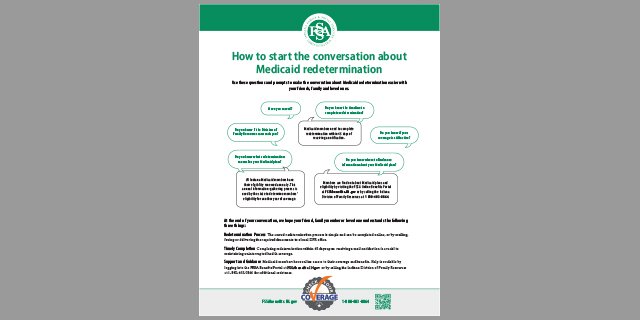
Your coverage under the Indiana Medicaid program will never be cut off without you first having the opportunity to give the state new and updated information. But it is important that you respond to requests from FSSA and provide the needed information when you’re contacted.
Planning documents and stakeholder meeting information
- Medicaid | End of Continuous Coverage Protections (June 2024)
- Medicaid | End of Continuous Coverage Protections (April 2024)
- Medicaid | End of Continuous Coverage Protections (Feb. 2024)
- Medicaid | End of Continuous Coverage Protections (Nov. 2023)
- Medicaid | End of Continuous Coverage Protections (Sept. 2023)
- Medicaid | End of Continuous Coverage Protections (Aug. 2023)
- Medicaid | End of Continuous Coverage Protections (June 2023)
- Medicaid | End of Continuous Coverage Protections (April 2023)
- Medicaid | End of Continuous Coverage Protections (March 2023)
- Medicaid | End of Continuous Coverage Protections (January 2023)
Outreach Materials
You can help by communicating to Hoosiers in your organization’s network about how the recent coverage protection changes will affect Indiana Medicaid members in April. Below are some resources to help you.
Other content
- Suggested messaging
- Help keep others informed. Click here to download a button to add to your website
- Protect your health. Protect your coverage – YouTube videos in English and Spanish
- Protect your health. Protect your coverage (English 60-sec)
- Protect your health. Protect your coverage (English 30-sec)
- Protect your health. Protect your coverage (English 15-sec)
- Protect your health. Protect your coverage (Spanish 60-sec)
- Protect your health. Protect your coverage (Spanish 30-sec)
- Protect your health. Protect your coverage (Spanish 15-sec)
- Keep your health coverage - Youtube videos in English
- Keep your health coverage (6 sec)
- Keep your health coverage (10 sec)
- Keep your health coverage (15 sec)
Sample Member Communications
The image above is an example of the envelope that mailed letters will arrive in.
- Initial letter: Potential changes to your health coverage
- Letter insert: Medicaid Eligibility Review Actions - The insert will be included in all notices sent to Medicaid members.
Sample packets sent to members the month of their redetermination
Members must complete packet and provide documentation to be considered for coverage
- IED426 – Must Return Asset Mailer - English and Spanish examples
- Sent to Aged/Blind/Disabled/Medicare Savings Program members
- This mailer may go to individuals who are only on Medicaid due to the public health emergency, or to members who have continued to meet all eligibility criteria throughout the public health emergency
- IED428 – Must Return Non-Asset Mailer - English and Spanish examples
- Sent to Healthy Indiana Plan and Hoosier Healthwise members
- This mailer may go to individuals who are only on Medicaid due to the public health emergency, or to members who have continued to meet all eligibility criteria throughout the public health emergency
- IED470 – COVID 19 Mailer – English and Spanish examples
- Sent to members if they are only on Medicaid due to the public health emergency and they are currently in a category that does not normally require annual redeterminations, but FSSA is unable to determine their continued eligibility in that category
- Example categories would be pregnant individuals who are past their 12th postpartum month, Social Security Insurance recipients, and foster care/adoption assistance/former foster care members who have aged out of those programs
Text messages sent to Medicaid members
Members will be receiving the messages below from the number 468311. They will receive three texts, five minutes apart, on the topic listed below. Members may opt out of receiving the texts at any time by replying STOP.
Topic: You should have received a redetermination packet messages:
- Message 1: Indiana Family & Social Services Administration has an update on your health coverage. Reply STOP at any time to stop receiving texts on this topic.
- Message 2: You should have received a redetermination packet that must be completed to determine if you are eligible. If you did not receive a packet, call 800-403-0864.
- Message 3: For more info on your health coverage, please click here: https://lnks.gd/2/22d6dTN
FSSA will not ask for any payment. Msg&Data rates may apply.
Automated phone call regarding missing redetermination forms
Members will receive automated phone calls from DFR requesting missing redeterminations forms. The phone calls with have the following message:
This is the Indiana Family and Social Services Administration, calling with an important message.
At this time, FSSA has not yet received redetermination paperwork for the Medicaid or HIP member whose benefit period is set to expire. However, if you return your documentation to FSSA, your benefits may remain open, if you qualify. Please review the notice you received about redetermination of your benefits and if you believe you still qualify for HIP or Medicaid this year, return your paperwork as soon as possible to FSSA. Redetermination packets can be completed online or uploaded to the benefits portal at fssabenefits.in.gov, or you can fax them to 800-403-0864, or mail them to FSSA Document Center, PO Box 1810, Marion, IN 46952. You can also drop them off at your local DFR office. If you did not receive your notice or you no longer have it, you can access a copy of the notice at FSSABenefits.in.gov. It will take a few days to process documents once they have been received by FSSA. If you have recently returned all of your redetermination paperwork, please disregard this message. If you have any questions, please call 800-403-0864, Monday through Friday, 8:00 AM to 4:30 PM.
If you would like to stop receiving phone calls from FSSA regarding important information on your case, please call 800-403-0864 and choose option 9 to opt out of the automated calling program.
Emails regarding missing redetermination forms
Members will receive an email from DFR requesting missing redetermination forms. The email will have the following subject and message:
FSSA Benefits Portal Important Information
At this time, FSSA has not yet received redetermination paperwork for the Medicaid or HIP member whose benefit period is set to expire. However, if you return your documentation to FSSA, your benefits may remain open, if you qualify. Please review the notice you received about redetermination of your benefits and if you believe you still qualify for HIP or Medicaid this year, return your paperwork as soon as possible to FSSA. Redetermination packets can be completed online or uploaded to the benefits portal at fssabenefits.in.gov, or you can fax them to 800-403-0864, or mail them to FSSA Document Center, PO Box 1810, Marion, IN, 46952. You can also drop them off at your local DFR office. If you did not receive your notice or you no longer have it, you can assess a copy at fssabenefits.ing.gov. It will take a few days to process documents once they have been received by FSSA. If you have recently returned all of your redetermination paperwork, please disregard this message. If you have any questions, please call 800-403-0864, Monday through Friday, 8:00 a.m. to 4:30 p.m.
Additional Resources
Agency portal
Agencies working with clients receiving public assistance through the Indiana Family and Social Services Administration’s Division of Family Resources often need to know whether a client has been approved for benefits. Once authorized, registered agencies may access the Agency Portal 24/7 to check the case status for each of the individuals they support. For more information or to sign up, please click here.
Electronic notices
Medicaid members can sign up for electronic notices through the Benefits Portal, available by clicking here. Individuals who have a Benefits Portal account can opt to receive an email notification when an eligibility notice or request for information has been generated for their case and then access the notice in the Benefits Portal. Members can also upload documents for FSSA using their online account, even if they have not opted into electronic notices.