Blood Lead Testing
Blood Lead testing is performed on children’s blood specimens for Pediatric Clinics, Head Start Programs, Day Care facilities and Local Health Departments around the state in support of the Indiana Lead and Healthy Homes Program (ILHHP). Initial screening is performed on finger stick blood specimens. Any Elevated Blood Lead Levels are verified using venous blood. Testing is free to the submitter.
Specimens are accepted for both Medicaid and non-Medicaid eligible patients. Any child or adult at risk for Lead Poisoning can be tested.
The IDOH Blood Lead Laboratory uses a sophisticated instrument called an Inductively Coupled Plasma / Mass Spectrometer (ICP/MS) for the accurate and sensitive detection of Lead in Blood specimens. The IDOH Laboratory does NOT use the Magellan LeadCare Analyzers.
HB1313
Effective Jan 1, 2023: Screening children for lead poisoning. Requires a health care provider who provides health care services to a child who is less than six years of age to take certain actions concerning a blood lead screening test from January 1, 2023, through December 31, 2026. Specifies that a parent or guardian is not required to have their child receive a blood lead screening test.
Blood Lead Specimen Collection and Submission Guidance
The Indiana Department of Health (IDOH) Laboratories sends participating providers collection supplies for capillary collection to include lancets, filter paper cards, alcohol prep pads, gauze, and bandages. In addition, the IDOH Containers Section at the Laboratories also will supply shipping containers for venipuncture confirmatory specimens. To order supplies, use the Laboratories online program - LimsNet.
LimsNet Access
To get to LimsNet, you first must have an Access Indiana account.
Use : Access Indiana | Sign In
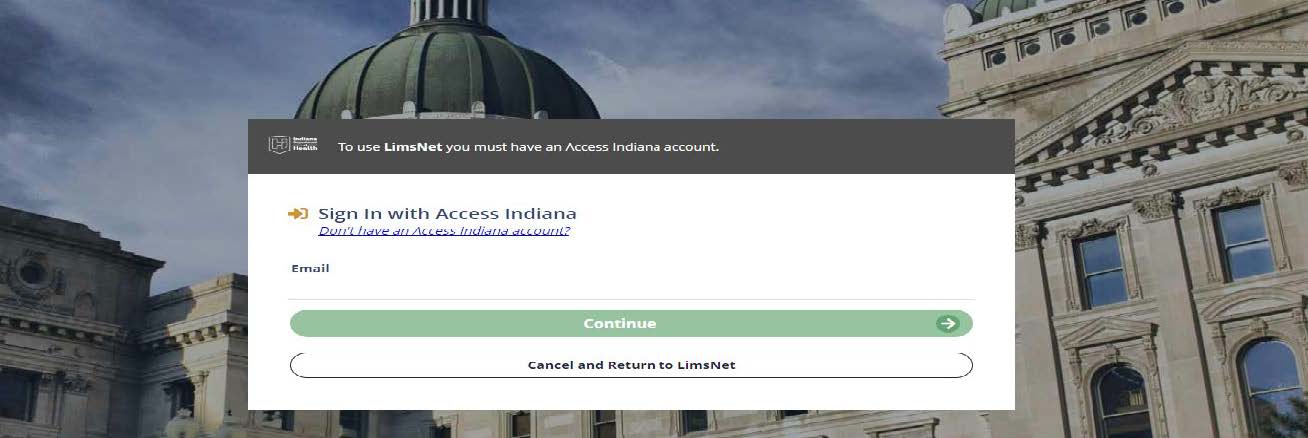 Figure 1
Figure 1
Choose LimsNet Tile
 Figure 2
Figure 2
To submit clinical specimens, you will still need an account associated with your facility. Contact LimsNet Help Desk: LimsAppSupport@health.IN.gov (email preferred) or 317-921-5506.
Filter Paper Cards (Dried Blood Spots)
- Identify patient.
- Cover clean work surface with paper towels from dust-proof box.
- Place the following items (Figure 3) on the paper towel for each child being tested:
- Gauze
- Alcohol wipe
- Lancet (blade style)
- Filter paper card
- Soap
- Powder-free gloves
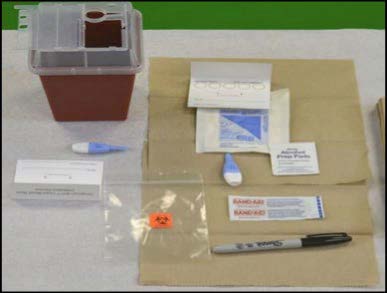 Figure 3
Figure 3
- Completely label filter paper card (Figure 4) with:
- Child’s full name
- Date of Birth
- Date of Collection
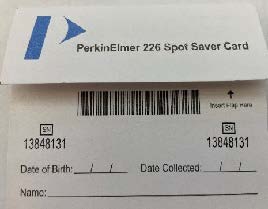

Figure 4
- Wash child’s hands with soap/water; dry with non-recycled paper towel from dust free box.
- Do not allow child to touch anything after washing.
- Open flap (if any) and lay flat.
- Do not touch any part of the filter paper or inside cover to avoid contamination.
- Do not fold flap under paper at this stage.
- Puncture finger with lancet. Pinky side of ring finger is a good choice.
- Wipe away first blood drop using gauze.
- Turn patient’s hand downward so finger is pointing to floor (Figure 5).
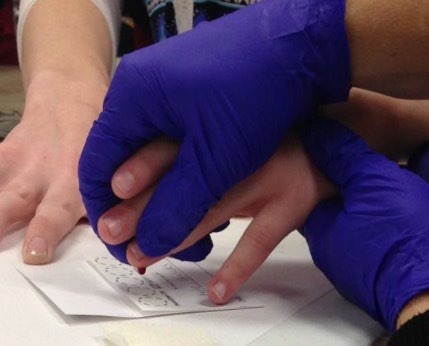 Figure 5
Figure 5
- Allow large drop to form at puncture site.
- Allow blood drop to free-fall onto collection card allowing card to absorb blood until circle is full.
- Do Not Touch Finger to Card.
- Minimum sample is 1 filled circle, but 2 is recommended (Figure 6).
- Place gauze on site and ask parent/guardian to hold pressure on finger.
- If necessary, bandage finger.
- Place filter paper on a drying rack (Figure 7), with the blood drops facing the ceiling. AVOID contact with blood drops.
- *Allow to dry for AT LEAST 4 hours away from direct sunlight or drafts from heat or air conditioning.
- A YouTube video is available at ISDH lab video.
 Figure 6 (1 spot minimum)
Figure 6 (1 spot minimum)
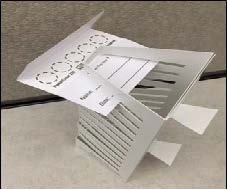 Figure 7
Figure 7
Microtainer Tubes
- Label microtainer tube.
- Wash child’s hands with soap/water; dry with paper towel from dust free box.
- Don’t let child touch anything after washing.
- Open cap of microtainer and lay on flat surface.
- Puncture finger with lancet. Pinky side of ring finger is a good choice.
- Wipe away first drop using gauze.
 Figure 8
Figure 8
- Turn patient’s hand downward such that the finger is pointing toward the floor.
- Allow large drop to form at puncture site (Figure 8).
- Allow blood drops to fall into microtainer tubes without scraping finger.
- Fill tube to first line (approximately 250 μL); do this within 2 minutes of puncture.
- Place gauze over site and ask parent/guardian to hold.
- Cap microtainer tube and invert immediately; this mixes the specimen to prevent clotting.
- Check labeling - show to parent/guardian for confirmation of correct information
- If necessary, bandage finger.
- Vacuum tube with EDTA preferred. These are not provided by IDOH. (Figure 9)
- Identify patient.
- Wash hands, tie tourniquet 3-4 inches above site (If it rolls up, it’s too tight).
- Have patient clench fist. Palpate veins in antecubital area.
- Loosen the tourniquet once a vein has been selected.
- Assemble your equipment, this may also be completed in the beginning.
- Tighten tourniquet again.
- Relocate vein and cleanse with 70% isopropyl alcohol.
- Allow alcohol to dry, less pain for patient this way.
- Place collection tube in tube holder (adapter).
- Remove needle cap.
- Turn needle to bevel up position.
- Pull skin taut just below puncture site.
- Insert needle at 30° angle (or less) (Figure 10).
- Insert quickly, but not so fast that you go through the vein.
- Do not weave needle into vein (like an IV start).
- You only need the bevel of needle in the vein to successfully draw blood (passing through the vein will cause a hematoma, or bleeding under the skin).
- Push tube into adapter while pulling on lip edges of adapter to allow smooth insertion of rear needle into collection tube.
- Allow tube to completely fill with blood.
- To remove tube: pull tube with fingers while pushing on adapter wings with thumb of same hand to allow smooth removal of collection tube from rear.
- Remove tourniquet (removing needle prior to removal of tourniquet can cause a hematoma).
- Place gauze over needle (without pushing down).
- Remove needle quickly, then apply pressure with gauze.
- Invert tube 5-7 times to mix.
- If patient is competent enough, ask them to hold pressure while you label the tube with the patient name, date of birth, date of collection.
- Hold for 1-2 min.
- Check to see if bleeding has stopped. This takes 5-10 seconds.
- Once bleeding has stopped, apply bandage.
- Application of bandage before bleeding has stopped can cause a hematoma.

 Figure 9
Figure 9
 Figure 10
Figure 10
Filter Paper (Dried Blood Spots)
- Place dried filter paper in plastic bags after drying.
- Put no more than 5-bagged samples in an envelope (Figure 11) for shipment to the IDOH Laboratories for testing.
- Include LimsNet Cover Sheet (Figure 12) with specimens.
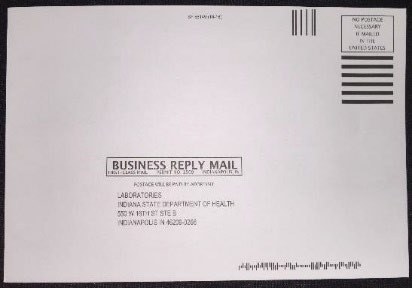 Figure 11
Figure 11
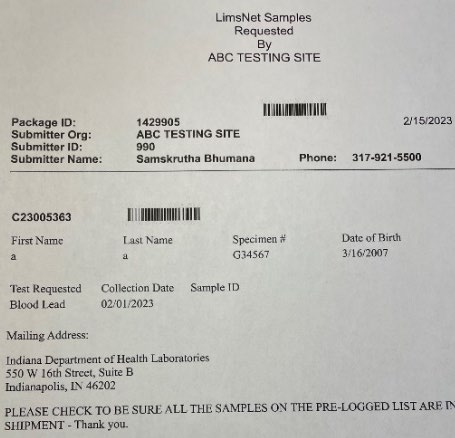 Figure 12
Figure 12
Capillary Microtainer Shipping
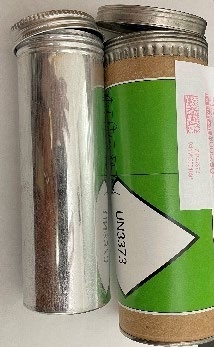
Figure 13
- Place completely labeled microtainer tubes in primary receptacle (Figure 13) with enough absorbent material to soak up all the liquid. Paper towels OK.
- Place paperwork and primary container in secondary receptacle.
- Label for UN3373 transport.
- Send to:
IDOH Laboratory
550 W. 16th Street
Suite B
Indianapolis, IN 46202
Attention: Blood Lead Laboratory
Venous Blood Tubes Shipping
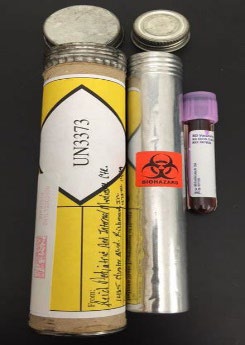
Figure 14
- Packaging (Figure 14) consists of the following components: primary receptacles (blood tubes not provided by IDOH Laboratories), and secondary packaging (materials used to protect primary blood tubes) required for UN3373 shipping.
- Place labeled venous tube in a leak-proof container or baggie.
- Place enough absorbent material to soak up all the liquid. Paper towels OK.
- Place primary container into secondary container. Tape Lid if it seems loose!
- Label for UN 3373 transport to:
IDOH Laboratory
550 W. 16th Street
Suite B
Indianapolis, IN 46202
Attention: Blood Lead Laboratory
Requesting Supplies
- Choose “Kit Order Blood Lead” from Log new order (Figure 15).
- Enter # pkgs requested.
- Click “Submit.”
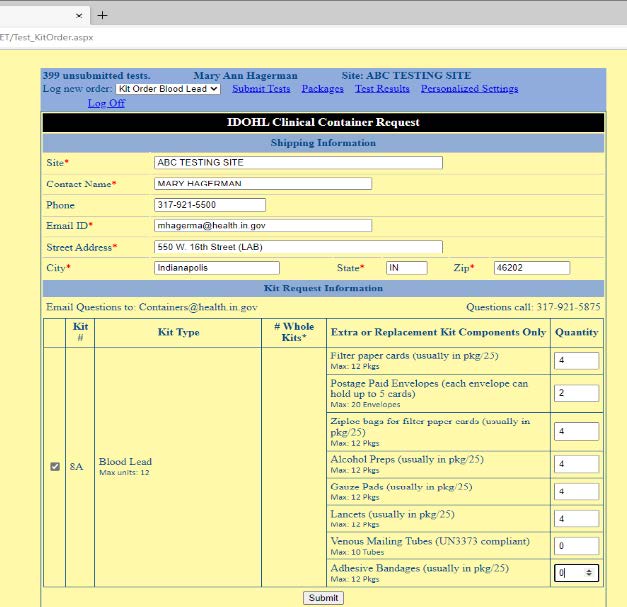 Figure 15
Figure 15
Enter Demographic Information
- Choose “Blood Lead.”
- Enter information. You must enter all the information marked with a red asterisk.
- Click on the Save button on the bottom of the page. You should get a message indicating the form has been successfully saved. If not, there is missing information or some error in entry! Please scroll up to review the form.
Marking Specimens to Ship to Laboratory
- Click on A Submit Tests at the top of the screen (Figure 16). You will see the saved entries ready to ship.
- Select the specimens you wish to ship B (remember-5 per envelope please).
- Click on C Submit Checked Samples at the bottom of the screen; a window should pop up with the cover page containing the package ID and corresponding barcodes for you to print and send with your specimens.
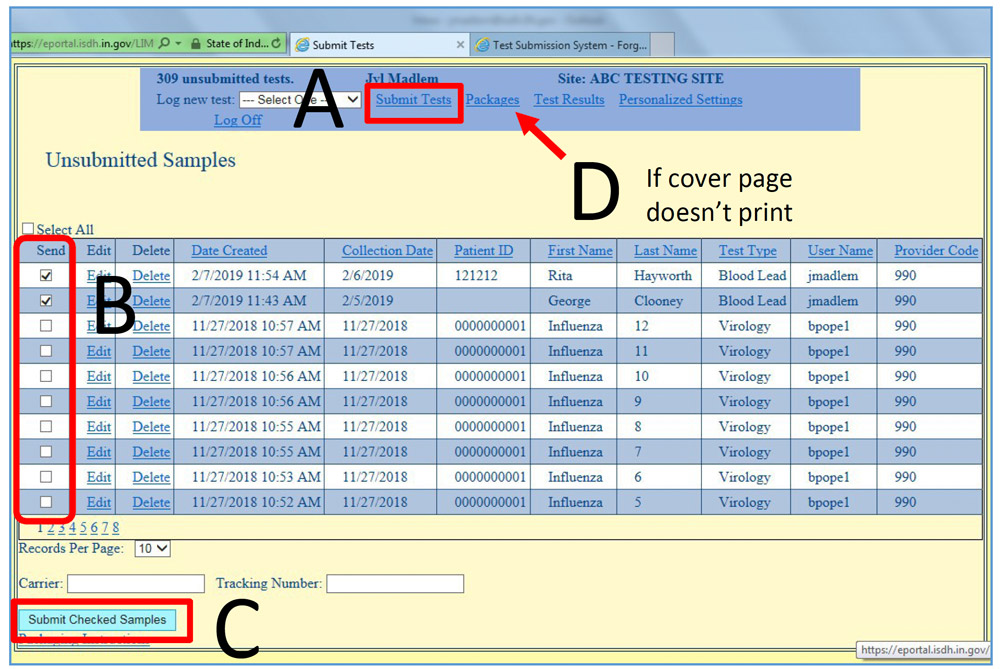 Figure 16
Figure 16
- NOTE: If your pop-up blocker is on, this cover page window will not open; you may do one of two things:
- Click on Packages (D above), which will direct you to a link to the cover page on the far right. Choose your package and select “Cover Page” (Figure 17).
- Turn off your pop-up blocker.
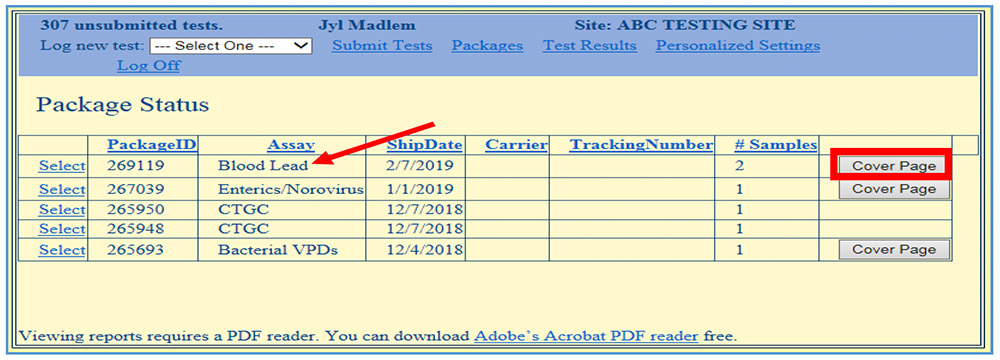 Figure 17
Figure 17
Chemistry Division Director
Mary Hagerman, MS
mhagerma@health.in.gov
317-921-5553
Laboratory Program Advisor
Janet Kent, MAFM, CT (ASCP)
jakent@health.in.gov
317-921-5574
Lead and Healthy Homes Division Program Manager
Sky Kolan
skolan@health.in.gov
317-234-2561
LimsNet Help Desk
LimsAppSupport@health.IN.gov (preferred)
or 317-921-5506
To set up an account, please email LIMSAppSupport@health.in.gov or call the help desk at 317-921-5506.
