Heart Disease
What is cardiovascular disease? What all falls under this label?
Cardiovascular disease, or other wise known as heart disease, can refer to a number of conditions. Heart disease may refer to conditions such as coronary artery disease, heart failure, heart valve problems, arrythmias and more. Just know heart disease is an umbrella term, and many conditions fall under this label.
- Heart disease is the leading cause of death for men, women, and people of most racial and ethnic groups
- One person dies every 33 seconds from cardiovascular disease
- In 2022, 702,880 people died from heart disease. That's the equivalent of 1 in every 5 deaths
- Heart disease cost about $252.2 billion from 2019 to 2020.This includes the cost of health care services, medicines, and lost productivity due to death.
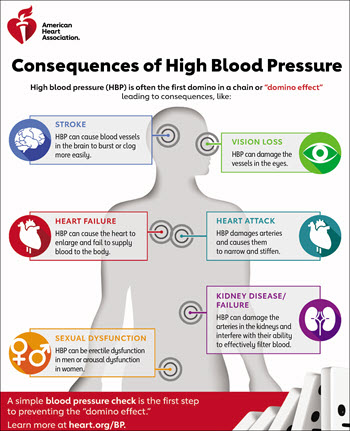
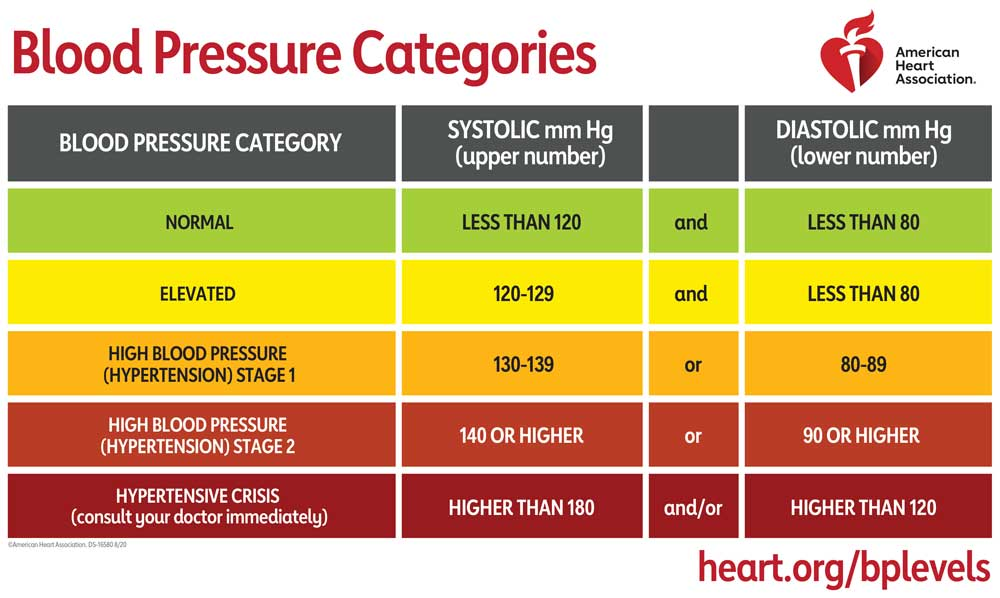
Blood pressure is a measure of the strength of blood pushing against the sides of the blood vessels in the circulatory system. Having high blood pressure is a risk factor for cardiovascular disease. Blood pressure is measured with two numbers. The top number, called systolic blood pressure, measures the pressure in the blood vessels when the heart beats. The bottom number, called diastolic blood pressure, measures the pressure in the blood vessels when the heart is at rest between beats. Blood pressure is measured in millimeters of Mercury (mm Hg).
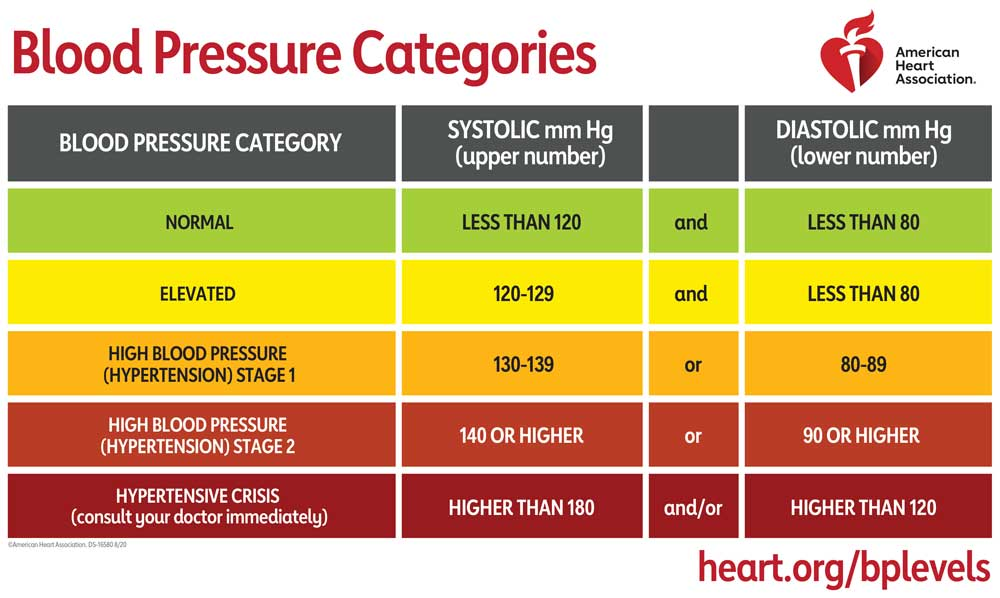
Measuring blood pressure regularly is the only way to know if blood pressure is high. At-home blood pressure machines are available at local pharmacies and retailers for purchase. There are also blood pressure machines available at pharmacies that can be used by patrons.
The American Heart Association recommends using an automatic, cuff-style, bicep (upper arm) monitor to measure blood pressure at home. Ask your doctor or pharmacist for advice or find options here and click here to read about home blood pressure monitoring.
When you are ready to take your blood pressure:
- Rest. Do not smoke, drink caffeine or exercise within 30 minutes of measurement.
Sit correctly. Sit in a chair with both feet flat on the floor. Sit next to a table to let your arm rest while you take your measurement. - Put on the cuff. Remove any tight clothing and place the cuff snugly around the upper part of your bare arm. The center of the cuff should sit over the artery.
- Be consistent. Take your blood pressure at the same time each day.
- Take multiple readings and record the results. Take two or three readings one minute apart, record the results, and share this at your next physician visit. If your monitor has built-in memory to store your readings, take it with you to your appointments. Some monitors may also allow you to upload your readings to a secure website after you register your profile.
- Don’t take your measurements over clothes.
- Record your results. Take two or three readings each time you take your blood pressure and record your results. Be sure to take your results to your next doctor’s appointment.
Monitoring Your Blood Pressure at Home
Measuring blood pressure regularly is the only way to know if blood pressure is high. At-home blood pressure machines are available at local pharmacies and retailers for purchase. There are also blood pressure machines available at pharmacies that can be used by patrons.
The American Heart Association recommends using an automatic, cuff-style, bicep (upper arm) monitor to measure blood pressure at home. Ask your doctor or pharmacist for advice or find options here and click here to read about home blood pressure monitoring.
When you are ready to take your blood pressure:
- Rest. Do not smoke, drink caffeine or exercise within 30 minutes of measurement.
Sit correctly. Sit in a chair with both feet flat on the floor. Sit next to a table to let your arm rest while you take your measurement. - Put on the cuff. Remove any tight clothing and place the cuff snugly around the upper part of your bare arm. The center of the cuff should sit over the artery.
- Be consistent. Take your blood pressure at the same time each day.
- Take multiple readings and record the results. Take two or three readings one minute apart, record the results, and share this at your next physician visit. If your monitor has built-in memory to store your readings, take it with you to your appointments. Some monitors may also allow you to upload your readings to a secure website after you register your profile.
- Don’t take your measurements over clothes.
- Record your results. Take two or three readings each time you take your blood pressure and record your results. Be sure to take your results to your next doctor’s appointment.
Percent Prevalence of High Blood Pressure, 2021
Prevalence of high blood pressure in Indiana: 31.85%
Hover a county for info
BRFSS Variable: Have you ever been told by a doctor, nurse or other health professional that you have high blood pressure? With response: Yes
Source: Indiana Behavioral Risk Factor Surveillance System
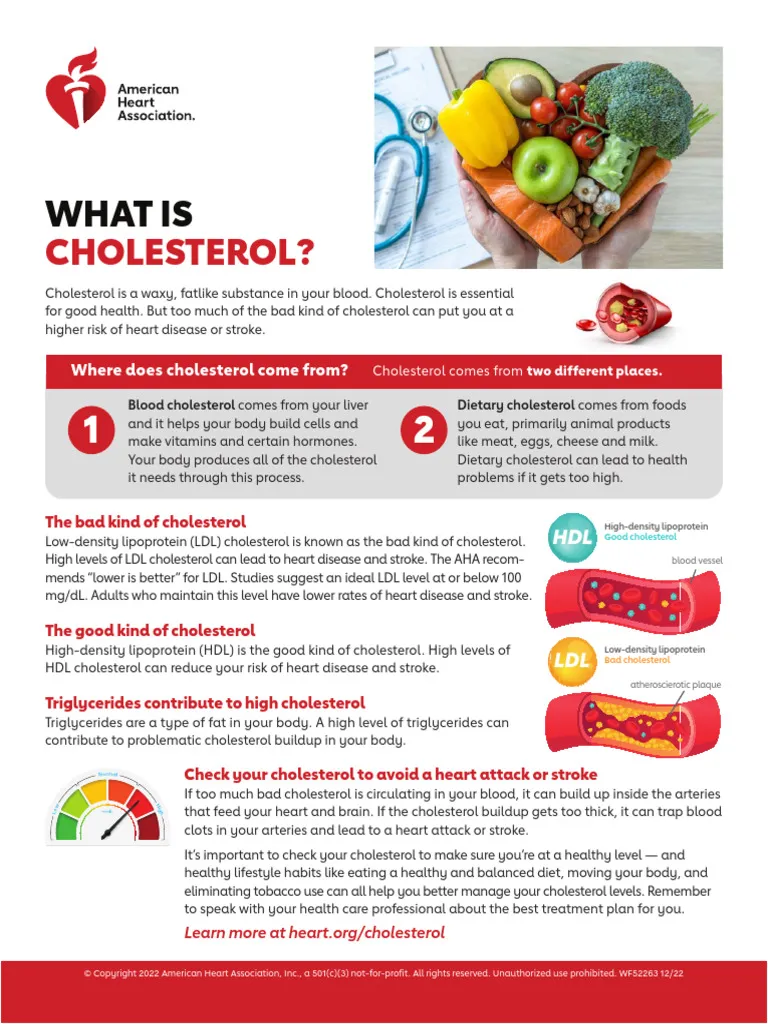
What is cholesterol and what does it do to your body?
Cholesterol is a waxy substance throughout the body. It’s not “bad” unless you have too much of it. Your body needs it to build cells and make vitamins and other hormones. But too much cholesterol can pose a problem. Cholesterol can join with other substances to form a thick, hard deposit on the inside of the arteries. This narrows the arteries and makes them less flexible – a condition known as atherosclerosis. Cholesterol comes from two sources. Your liver makes all the cholesterol you need. The remainder of the cholesterol in your body comes from foods from animals. For example, meat, poultry and dairy products all contain dietary cholesterol. Behaviors that can negatively affect your cholesterol levels include Unhealthy diet, Lack of physical activity, Smoking or exposure to tobacco smoke, Being overweight or obese. Some people inherit genes from their mother or father that cause them to have too much cholesterol. This is called familial hypercholesterolemia (FH). The severity of FH is related to the duration and degree of LDL cholesterol in the blood. FH is dangerous because it can cause premature atherosclerotic heart disease.
Percent Prevalence of High Cholesterol, 2021
Prevalence of high cholesterol in Indiana: 30.45%
Hover a county for info
BRFSS Variable: Have you ever been told by a doctor, nurse or other health professional that your cholesterol is high? With response: Yes
Source: Indiana Behavioral Risk Factor Surveillance System
- Coronary Artery Disease
- Treatment for Coronary Artery Disease
- Angina
- Heart Failure
- Heart Attack
- Arrthythmia
- Atrial Fibrillation
Coronary Artery Disease
Coronary artery disease also known as coronary heart disease is caused by the build-up of plaque in the arteries that supply oxygen-rich blood to the heart. Plaque, a mixture of fat, cholesterol, and calcium deposits, can build up in the arteries over many years.
Over time, this plaque can cause the narrowing and hardening of the coronary arteries, a condition called atherosclerosis.
Coronary artery disease can often be symptom-free, but people with coronary artery disease have an increased risk of angina (chest pain or discomfort), heart attack, heart failure, and cardiac arrhythmias.
- Coronary heart disease is the most common type of heart disease. It killed 371,506 people in 2022
- About 1 in 20 adults age 20 and older have CAD (about 5%)
- In 2022, about 1 out of every 5 deaths from cardiovascular diseases (CVDs) was among adults younger than 65 years old
If you have coronary artery disease, there are steps you can take to lower your risk for having a heart attack or worsening heart disease. Your doctor may recommend lifestyle changes such as eating a healthier diet, exercising, and not smoking.
Medications may also be necessary. Medicines can treat coronary artery disease risk factors such as high cholesterol, high blood pressure, an irregular heartbeat, and low blood flow. In some cases, more advanced treatments and surgical procedures can help restore blood flow to the heart.
Learn more:
Angina, or chest pain and discomfort, is the most common symptom of CAD. Angina can happen when too much plaque builds up inside arteries, causing them to narrow. Narrowed arteries can cause chest pain because they can block blood flow to your heart muscle and the rest of your body.
To learn more about Angina visit these websites:
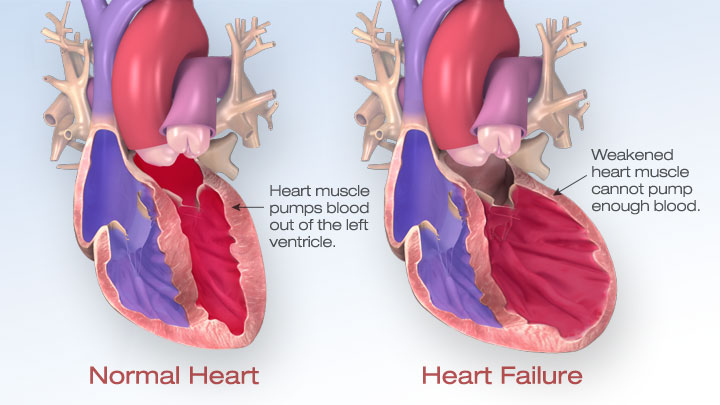
Heart Failure occurs when the heart cannot pump enough blood and oxygen to support other organs. Heart failure is a serious condition, but it does not mean that the heart has stopped beating.
The most common causes of heart failure are coronary artery disease, high blood pressure, and diabetes.
- In the United States, nearly 6.7 million adults 20 years old or older have heart failure.1
- In 2022, heart failure was mentioned on 457,212 death certificates (and responsible for 13.9% of all causes of death).2
- Heart failure cost the nation an estimated $30.7 billion in 2012. This total includes the cost of health care services, medicines to treat heart failure, and missed days of work.3
Early diagnosis and treatment can improve quality of life and life expectancy for people who have heart failure. Treatment usually involves taking medicines, reducing salt in the diet, and getting daily physical activity. People with heart failure also track their daily symptoms and discuss them with their doctors.
Common symptoms of heart failure include:
- Shortness of breath during daily activities.
- Having trouble breathing when lying down.
- Weight gain with swelling in the legs, ankles, or lower back.
- General fatigue and weakness.
Lean More
A heart attack, also known as a myocardial infarction, happens when the flow of blood that brings oxygen to a part of your heart muscle suddenly becomes blocked. Your heart can’t get enough oxygen. If blood flow is not restored quickly, the heart muscle will begin to die.” This is different from a cardiac arrest. “Cardiac arrest occurs when the heart suddenly and unexpectedly stops pumping. If this happens, blood stops flowing to the brain and other vital organs. Cardiac arrests are caused by certain types of arrythmias (or an irregular heartbeat) that prevent the heart from pumping blood.” Sudden cardiac arrest is caused by an electrical problem.
- In the United States, someone has a heart attack every 40 seconds
- Every year, about 805,000 people in the United States have a heart attack. Of these, 605,000 are a first heart attack, and 200,000 happen to be people who have already had a heart attack
- About 1 in 5 heart attacks are silent—the damage is done, but the person is not aware of it
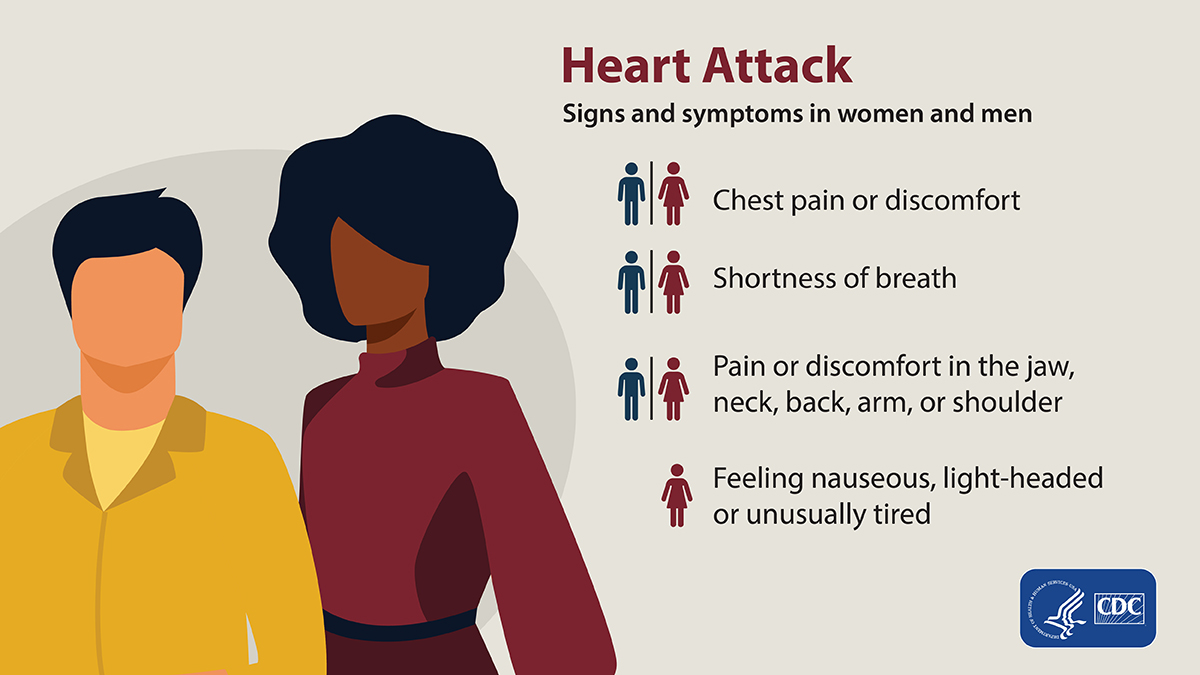
The major symptoms of a heart attack are:
- Chest pain or discomfort. Most heart attacks involve discomfort in the center or left side of the chest that lasts for more than a few minutes or that goes away and comes back. The discomfort can feel like uncomfortable pressure, squeezing, fullness, or pain.
- Feeling weak, light-headed, or faint. You may also break into a cold sweat.
- Pain or discomfort in the jaw, neck, or back.
- Pain or discomfort in one or both arms or shoulders.
- Shortness of breath. This often comes along with chest discomfort, but shortness of breath also can happen before chest discomfort.
Other symptoms of a heart attack could include unusual or unexplained tiredness and nausea or vomiting. Women are more likely to have these other symptoms.
Arrhythmias (ah-RITH-me-ah) are irregular, or abnormally fast or slow, heartbeats. Some arrhythmias are serious. One example is ventricular fibrillation. This type of arrhythmia causes a severely abnormal heart rhythm that leads to death unless treated right away with an electrical shock to the heart (called defibrillation). Other arrhythmias are less severe, but can develop into more serious conditions such as atrial fibrillation.
Atrial fibrillation, often called AFib or AF, is the most common type of treated heart arrhythmia. An arrhythmia is when the heart beats too slowly, too fast, or in an irregular way.
When a person has AFib, the normal beating in the upper chambers of the heart (the two atria) is irregular, and blood doesn't flow as well as it should from the atria to the lower chambers of the heart (the two ventricles). AFib may happen in brief episodes, or it may be a permanent condition.
- It is estimated that 12.1 million people in the US will have AFib
- In 2021, AFib was mentioned on 232,030 death certificates and was the underlying cause of death in 28,037 of those deaths
- People of European descent are more likely to have AFib than Black people
- Because the number of AFib cases increases with age and women generally live longer than men, more women than men experience AFib
How is AFib related to stroke?
AFib increases a person's risk for stroke. When standard stroke risk factors were accounted for, AFib was associated with an approximately fivefold increased risk of ischemic stroke.6 AFib causes about 1 in 7 strokes.7
Strokes caused by complications from AFib tend to be more severe than strokes with other underlying causes. Strokes happen when blood flow to the brain is blocked by a blood clot or by fatty deposits called plaque in the blood vessel lining.
Learn more:
- Symptoms of heart attack
The major symptoms of a heart attack are:
- Chest pain or discomfort. Most heart attacks involve discomfort in the center or left side of the chest that lasts for more than a few minutes or that goes away and comes back. The discomfort can feel like uncomfortable pressure, squeezing, fullness, or pain.
- Feeling weak, light-headed, or faint. You may also break into a cold sweat.
- Pain or discomfort in the jaw, neck, or back.
- Pain or discomfort in one or both arms or shoulders.
- Shortness of breath. This often comes along with chest discomfort, but shortness of breath also can happen before chest discomfort.
Other symptoms of a heart attack could include unusual or unexplained tiredness and nausea or vomiting. Women are more likely to have these other symptoms.
- Arrhythmia
Arrhythmias (ah-RITH-me-ah) are irregular, or abnormally fast or slow, heartbeats. Some arrhythmias are serious. One example is ventricular fibrillation. This type of arrhythmia causes a severely abnormal heart rhythm that leads to death unless treated right away with an electrical shock to the heart (called defibrillation). Other arrhythmias are less severe, but can develop into more serious conditions such as atrial fibrillation.
- Atrial Fibrillation
Atrial fibrillation, often called AFib or AF, is the most common type of treated heart arrhythmia. An arrhythmia is when the heart beats too slowly, too fast, or in an irregular way.
When a person has AFib, the normal beating in the upper chambers of the heart (the two atria) is irregular, and blood doesn't flow as well as it should from the atria to the lower chambers of the heart (the two ventricles). AFib may happen in brief episodes, or it may be a permanent condition.
- It is estimated that 12.1 million people in the US will have AFib in S12
- In 2021, AFib was mentioned on 232,030 death certificates and was the underlying cause of death in 28,037 of those deaths.3
- People of European descent are more likely to have AFib than Black people.
- Because the number of AFib cases increases with age and women generally live longer than men, more women than men experience AFib.
How is AFib related to stroke?
AFib increases a person's risk for stroke. When standard stroke risk factors were accounted for, AFib was associated with an approximately fivefold increased risk of ischemic stroke.6 AFib causes about 1 in 7 strokes.7
Strokes caused by complications from AFib tend to be more severe than strokes with other underlying causes. Strokes happen when blood flow to the brain is blocked by a blood clot or by fatty deposits called plaque in the blood vessel lining.
- Learn more about arrhythmia
What does treatment and recovery look like for heart disease? With the variety of things that fall under heart disease come a variety of treatment options. One common recovery option for many aspects of heart disease is cardiac rehab. “Cardiac rehab is a medically supervised program designed to improve your cardiovascular health.” Cardiac rehab will help with exercise counseling and training, heart-healthy lifestyle education, and will help you try to reduce your stress. Physical activity and exercise play a major role in the prevention, management, and treatment of heart disease. Ask your doctor if you are eligible for cardiac rehab. For specific information on things like heart failure, arrythmias, artery diseases, and the treatments and procedures for each please visit: What is Cardiovascular Disease? | American Heart Association
Sources:
- CDC Heart Disease, accessed October 23, 2024